What Is Thumb Arthritis?
Any condition that irritates or destroys a joint is referred to as arthritis. Over 100 types afflict the human body, and thumb arthritis is a painful form of this condition.
By far, osteoarthritis, or degenerative joint disease, is the most common cause of arthritis-related thumb pain. In a normal joint, cartilage covers the ends of articulating bones and permits their smooth, painless movement against one another.
In osteoarthritis, the cartilage layer wears out, allowing bone to contact against bone. As this process destroys the joint, the signs and symptoms of arthritis develop.
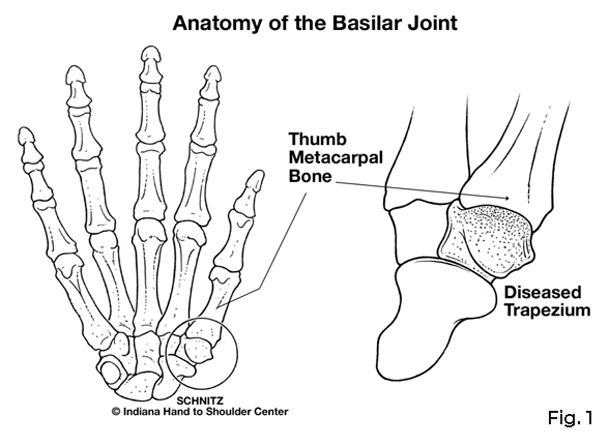
The basilar joint, or the first carpometacarpal joint of the thumb, is formed by a small wrist bone called the trapezium and the thumb metacarpal bone. (Fig. 1)
The unique shapes of these bones permit the thumb to move in and out of the plane of the palm, as well as bend across the palm to oppose the other fingers.
Thumb arthritis involving the base of the thumb is far more common in women than men and typically occurs after age 40. A prior history of fracture or other injuries to the joint may increase the likelihood of developing arthritis
What Are the Signs and Symptoms?
The earliest symptom of thumb arthritis is pain with activities that involve pinch. These include opening jars, doorknobs, car doors, and turning keys. Prolonged or heavy use of the thumb may produce an aching discomfort at the base of the thumb.
Changes in the weather may produce similar symptoms. As the disease progresses, less stress is required to produce the pain. Pinch strength diminishes. Activity-related swelling may develop.
Later, any motion of the thumb, even without stress, may become painful. Eventually, the joint begins to appear enlarged and out of place. This is usually accompanied by limited thumb motion.
The amount of functional loss to the thumb may vary as the disease progresses. Early on, the motion of the thumb is normal. Later, however, motion becomes impaired. The most challenging maneuver is often pulling the thumb away from the hand to reach around an object.
In severe cases, the thumb metacarpal collapses into the palm, and other joints may assume an abnormal position to permit a wider grasp.
How Is the Diagnosis Made?
A careful history will frequently alert the physician to suspect thumb arthritis. Inspection of the thumb will sometimes reveal a tender prominence at the base of the thumb that represents either inflammation of the joint or displacement of the thumb metacarpal.
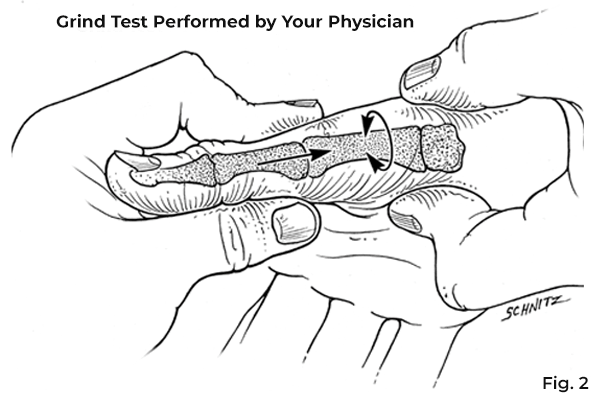
Your physician may press the thumb metacarpal firmly against the trapezium and move the joint as a diagnostic measure. This grind test usually produces pain symptoms and may produce a gritty sensation called joint crepitance. (Fig. 2)
This represents bone contact against bone, which may also appear on an x-ray.
How Is Thumb Arthritis Treated?
Initially, the symptoms may respond to limited activities and rest. If this fails, anti-inflammatory medication and a protective splint may be of benefit.
Additional relief of thumb arthritis symptoms can sometimes be achieved by a cortisone injection into the joint. When conservative treatment methods no longer help, surgery may be warranted.
If Surgery Is Necessary
The goal of surgery is to decrease pain and preserve motion in the thumb. This is accomplished by removing the destroyed joint and creating a substitute joint called an arthroplasty. (Fig. 3)
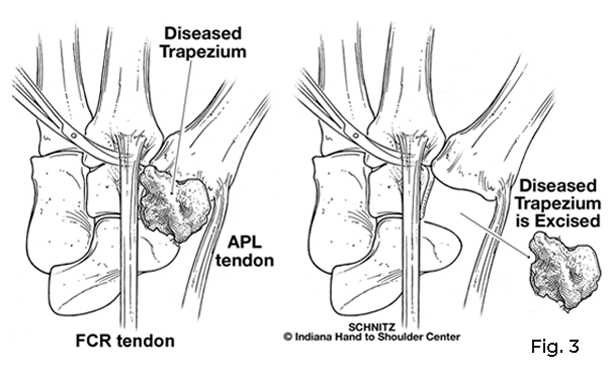
All or part of the trapezium is replaced with either an artificial substance or a strip of the tendon to create a sling suspension. The procedure can be performed on an outpatient basis and requires either a regional block or general anesthetic.
A small stainless steel pin may be used to temporarily stabilize the reconstructed joint.
What to Expect Following Surgery
Following surgery for thumb arthritis, the hand is immobilized in a bulky compressive dressing with a rigid splint to protect the thumb. The fingers are usually left free to permit early motion.
Elevation of the entire upper extremity and movement of the fingers is significant to prevent undesired swelling. Although the fingers and tip of the thumb are free, the hand is generally unable to do normal daily activities in the bulky dressing. The postoperative dressing is changed, and sutures are removed ten to 14 days after surgery.
A splint or cast will next be applied for an additional two to four weeks of immobilization.
Approximately four to six weeks following surgery, a therapy program is initiated to restore motion to the thumb. (Fig. 4)
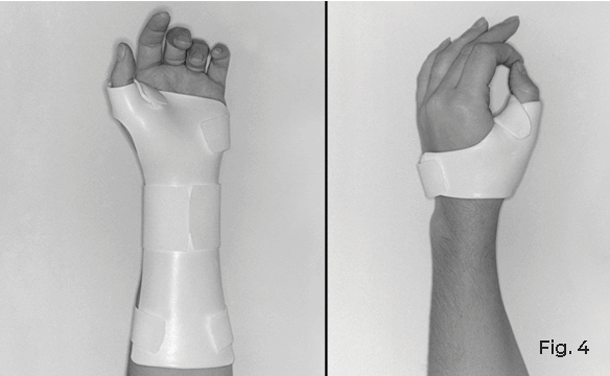
The fixation pin, if used, is removed at this time. A small splint is made to protect the thumb between exercises and maintain the web space between the thumb and index finger.
A therapist will provide a specific exercise program and advice on what activities are allowed. Discomfort with early therapy is not uncommon and improves with time.
Unrestricted use of the thumb is usually permissible at 12 weeks after surgery. Up to one year may be required before the maximum benefits of surgery are achieved.
No part of this work may be reproduced without written permission from the Indiana Hand to Shoulder Center.
Disclaimer: The materials on this website have been prepared for informational purposes only and do not constitute advice. You should not act or rely upon any medical information on this website without a physician’s advice. The information contained within this website is not intended to serve as a substitution for a thorough examination from a qualified healthcare provider. The display of this information is not intended to create a health care provider-patient relationship between the Indiana Hand to Shoulder Center and you.
Thumb Arthritis Patient Handout
